Researchers supported by the NIHR Oxford Biomedical Research Centre (BRC) have studied the link between people diagnosed with COVID-19 as outpatients and the short-term risk of developing blood clots, and the clinical and genetic risk factors that predispose them to developing post–COVID-19 thrombosis.
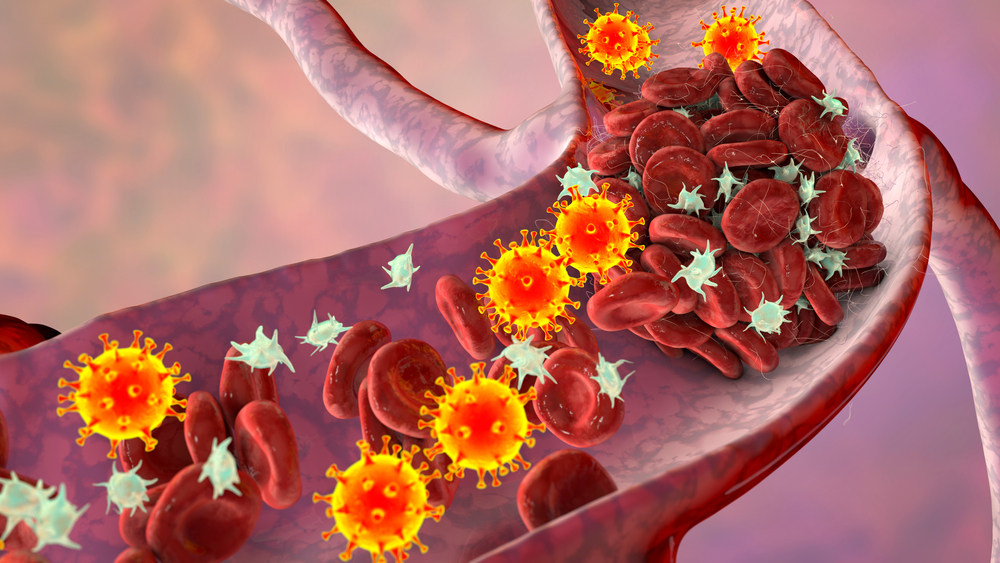
Ambulatory COVID-19 patients (those diagnosed as outpatients) face an increased risk of venal thrombosis (blood clot in a vein) than the general population not affected by COVID-19, according to a new study by University of Oxford researchers.
But the researchers from the Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences (NDORMS) found that the risk was greatly reduced in fully vaccinated people with breakthrough infection.
Published in JAMA Internal Medicine, the retrospective, population-based cohort study examined the records of more than 400,000 participants from the UK Biobank. Some 18,818 were infected with SARS-CoV-2, identified by a positive PCR test in community settings. These were matched against 93,179 uninfected participants according to age, gender and a series of clinical features.
Frank Xie, lead author and research assistant in pharmaco-epidemiology at NDORMS, said: “Numerous hospital-based studies have demonstrated VTE (venous thromboembolism, or blood clots) in patients with severe COVID-19 who have been admitted for treatment. This was one of the first studies into ambulatory patients with the virus, and we’ve found that there is a substantially increased risk of VTE among this cohort of middle age and older patients.”
Other clinical risk factors include older age, being male, and obesity.
The team also identified genetic factors that predisposed patients to VTE. Those who carry the Factor V Leiden genetic mutation – which can result in an increased tendency to form abnormal blood clots – had an additional double risk of post–COVID-19 VTE compared with those without the mutation. This is equivalent to the excess risk associated with being ten years older,
“We did, however, find that the risk was significantly decreased for individuals who had been fully vaccinated,” said Frank. “Reinforcing the need for vaccinations, these findings may help to turn the tide of vaccine hesitancy and restrictions on their use. It could also help healthcare providers re-evaluate how they attentively prioritise treatments such as prophylaxis for milder ambulatory COVID-19 patients to mitigate the risks of VTE.”