Unequal access to early pregnancy scans delays detection of serious conditions. Early screening resulted in earlier detection for 40% of anomalies, including heart and limb issues. Researchers from the University of Oxford, supported by NIHR Oxford Biomedical Research Centre, together with colleagues from the NHS and other partners, have published the first population-level study linking first-trimester ultrasound practice with early detection rates for serious congenital anomalies.

“Impact of first trimester ultrasound on early detection of major fetal anomalies”, published in PLOS Medicine, is the first study to analyse national data linking first-trimester ultrasound protocols to detection rates for serious congenital anomalies.
Analysing more than 1 million pregnancies across England, the study found that NHS trusts using the most detailed early screening protocols detected 40% of major fetal anomalies before 16 weeks, compared with 28% in trusts with no formal anatomical assessment at this stage.
The findings have significant implications for national screening policy, parental decision-making, and equity of care. Despite technological advances making early detection possible, there is no national policy recommending first-trimester anatomical screening in England, leading to striking regional differences in practice.
Major Findings:
- Three-quarters of NHS trusts currently conduct first-trimester anatomical screenings, but what is assessed varies greatly.
- More detailed protocols were associated with substantially higher early detection rates for conditions such as spina bifida, major heart defects, and limb abnormalities.
- Some conditions (including acrania, exomphalos, and gastroschisis) were frequently detected early regardless of policy, while other conditions remained hard to detect before 16 weeks, even with detailed scanning.
- Significant regional variation means a woman’s chance of early detection depends heavily on where she lives.
Policy and clinical implications:
Earlier diagnosis allows more time for further investigations, multidisciplinary care planning, consideration of in-utero treatment options, and informed parental decisions. It can also reduce the health risks associated with later interventions.
Researchers say the evidence now strongly supports consideration of nationally standardised first-trimester screening protocols to ensure all pregnant women have equal access to early detection, regardless of postcode.
Lead researcher, Dr Jehan Karim, said, “With advancing ultrasound technology, much earlier detection of serious fetal conditions is now feasible; our guidance must catch up to these developments so families can benefit.”
Author lead, Prof Aris Papageorghiou adds “A single, focussed first-trimester ultrasound scan brings the diagnosis of major fetal conditions forward by weeks; this gives families time to consider and expand clinical options. However, the lack of guidance has led to variation in practice. Our findings are clear: an organised first-trimester scan is the most effective step to improve prenatal detection across the NHS.”
The research methods:
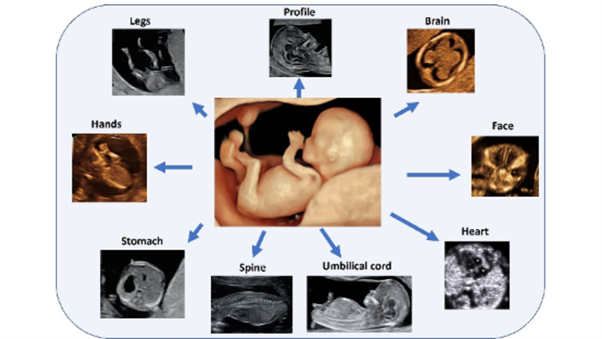
The research team linked results from a national survey of first-trimester ultrasound protocols across all NHS maternity units in England with data from the National Congenital Anomaly and Rare Disease Registration Service (NCARDRS) for pregnancies between April 2017 and March 2019. NHS trusts were grouped by the level of anatomical detail in their first-trimester scans: no protocol, basic, advanced, or extended. The study then compared rates of early detection for 14 major congenital anomalies, including serious heart defects, spina bifida, limb reduction defects, and abdominal wall defects.
The research was a collaboration between:
- Nuffield Department of Women’s & Reproductive Health, University of Oxford
- National Congenital Anomaly and Rare Disease Registration Service (NCARDRS), NHS England
- NHS Fetal Anomaly Screening Programme, NHS England
- Fetal Medicine Unit, University College London Hospitals NHS Foundation Trust
- Oxford Maternal and Perinatal Health Institute, Green Templeton College, University of Oxford
AS well as the NIHR Oxford BRC, the study was funded by the National Institute for Health Research (NIHR) Health Technology Assessment board.