Scientists at the University of Oxford, have identified how rare populations of abnormal cells drive the formation and persistence of fistulas – painful, tunnel-like tracts that develop in around 30% of people with Crohn’s disease.
Crohn’s disease is a long-term disease that affects around one in every 650 people, in which parts of the gut become swollen, inflamed and ulcerated. When ulcers or inflammation in the intestinal wall fail to heal properly, Crohn’s fistulas can form, burrowing into surrounding tissue and sometimes connecting to other organs or the skin. Precisely how these form, grow and persist has remained unclear and they are very challenging to treat.
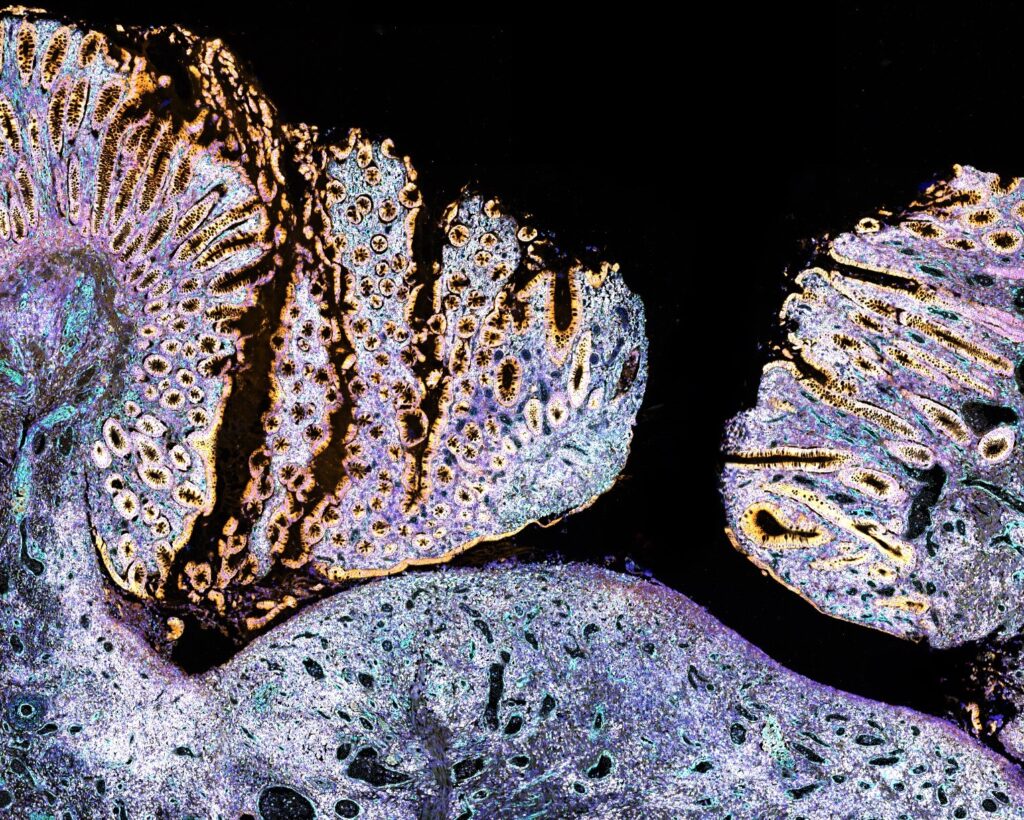
In this study, published in Nature, researchers analysed thousands of individual cells from Crohn’s fistulas, comparing them with healthy gut tissue. Using advanced single-cell and spatial analysis techniques, the team at the MRC Weatherall Institute of Molecular Medicine, supported by the NIHR Oxford Biomedical Research Centre, mapped the precise composition and behaviour of cells within the fistula tracts.
They discovered that fistulas are lined by concentric rings of “rogue” fibroblasts – cells that normally maintain tissue structure – that have become reprogrammed to act like cells involved in early fetal gut development. This out-of-context activity caused fibroblasts near the tract surface to destroy the surrounding tissue, promoting tunnelling, while deeper fibroblasts produced stiff, fibrotic material that stabilised and maintained the tunnels.
“These fibroblasts have essentially switched on developmental programmes that should only be active before birth,” said Dr Agne Antanaviciute, one of the senior authors. “This reawakening makes them highly destructive. They erode tissue at the surface and lay down fibrotic scar deeper in the tract, helping the tunnels form and persist.”
Traces of these abnormal fibroblasts were also found in small numbers at the bases of ulcers in Crohn’s patients who had not yet developed fistulas. This finding suggested that early intervention to modulate local signalling could prevent tunnel formation altogether.
Professor Alison Simmons, senior author and Director of the MRC Translational Immune Discovery Unit, said: “Current medicines for Crohn’s, and other types of inflammatory bowel disease (IBD), focus on suppressing inflammation, but do little to promote tissue repair. By pinpointing the cell types and pathways that actually drive fistula formation, we now have more of the vital information required to design and test preventatives and novel wound healing approaches.”
The Oxford team’s work produced the largest-ever dataset of its kind, integrating single-cell, spatial and molecular imaging data across diverse patient samples. All data have been made publicly available to accelerate global research into Crohn’s complications.
The findings provide a new foundation for drug discovery aimed at restoring healthy cell communication and wound healing within the gut; a crucial step toward therapies that can prevent or reverse one of the most devastating aspects of Crohn’s disease.
Clinical researcher Colleen McGregor, co-first author of the study, said: “As a clinician who sees first-hand the burden of this debilitating complication, I’m thrilled to have helped define key aspects of fistula biology – an area where data have long been limited.
“This work exemplifies the power of interdisciplinary analysis at the interface of clinical medicine and science – the foundation of high-quality IBD care.”
As well as the Oxford BRC, this research was supported by the UKRI Medical Research Council, the Leona M. and Harry B. Helmsley Charitable Trust and the Wellcome Trust.