Researchers from the University of Oxford, working with Public Health England, have used NHS Test and Trace data to find out why some individuals pass COVID-19 on to their contacts more easily than others, and if lateral flow tests are sufficient in detecting those who are most infectious.
Using information from over a quarter of a million people who have participated in the UK government’s Test and Trace programme, the scientists, who are supported by the NIHR Oxford BRC, found that in all groups, the more virus detected in the nose and throat (known as ‘viral load’), the more infectious the individual is.
This is the first time this has been confirmed in a large-scale study and explains, in part, why some people pass COVID-19 on and others do not. Overall, only six in 100 contacts of infected cases went on to get infected themselves.
Understanding why some individuals with COVID-19 are more infectious than others has been a key piece of information missing from creating a more effective testing system. Since those with higher viral loads are more likely to pass the infection on to others, these infected individuals are the most important to detect, so they can be isolated, thus reducing onward transmission.
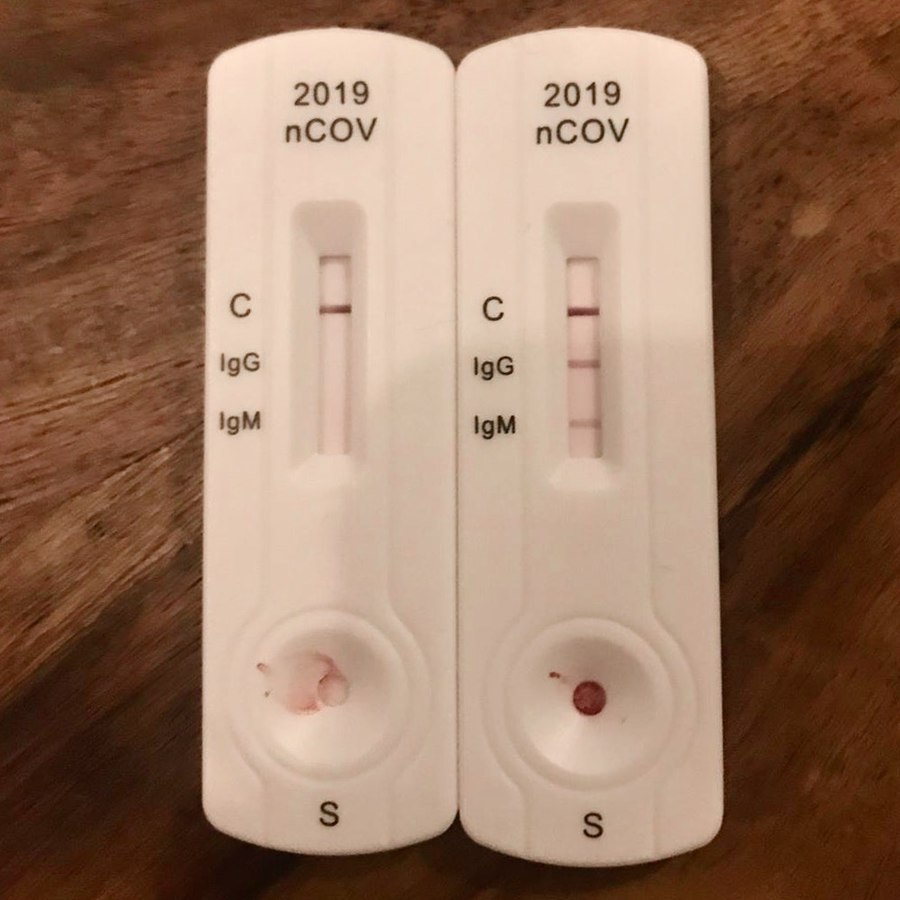
COVID-19 tests that are less sensitive than the standard PCR but easier to make widely available, such as lateral flow tests, could be a good solution to ensuring those who are highly infectious are able to know they need to isolate more quickly and could allow an easing of lockdown restrictions.
They would also allow more people to be tested, yielding immediate results, including those who do not have symptoms and people at increased risk of testing positive, for example, because of their work or having been a contact themselves.
Tim Peto, Professor of Medicine at the University of Oxford and senior author on the study, said: “Lateral flow tests have been very popular with staff at our hospitals in Oxford, with over 60,000 tests done since November. We’ve been able to detect asymptomatic infected staff who would not have been otherwise diagnosed, protecting patients and staff. The tests can be done at home before coming to work with a result available within 30 minutes.”
Although lateral flow tests are a rapid and relatively cheap way to detect COVID-19, their role in detecting actively infectious people has been controversial. While lateral flow tests do not detect as many cases as the standard PCR test, there has been much debate on whether they are ‘good enough’ to catch most infectious cases of COVID-19.
It was already known that lateral flow tests are more accurate the more virus is present. Because this research has shown that the same people who are detected best by lateral flow kits, with high viral loads, are also the most infectious, this means that lateral flow tests can detect most people who would otherwise go on to infect someone else.
In the current research, modelling has found that they would be effective at detecting up to 90% of the infections that the individuals then passed on to their contacts.
Summarising the findings, Prof Peto said: “We know that lateral flow tests are not perfect, but that doesn’t stop them being a game changer for helping to detect large numbers of infectious cases sufficiently rapidly to prevent further onward spread.”
As well as investigating if lateral flow tests could prevent transmission, the researchers also investigated what sorts of contact and which people were most likely to spread COVID-19. They found that contacts in the same household were more likely to become infected than contacts at work, school or elsewhere. Children were less likely to infect someone else. Among household visitors, those in their 20s and over 65 years were more infectious.
Dr David Eyre, of Oxford’s Big Data Institute and Nuffield Department of Population Health and an Oxford BRC Senior Research Fellow, co-led the study. He said: “When the time comes to relax the current lockdown restrictions, by rapidly identifying the most infectious people using these lateral flow tests, we can potentially relax the lockdown much more safely. This would allow people to get back to work, school and their normal activities and still stay safe.”