A University of Oxford research team has used single-cell technology to identify new players in the gut epithelial barrier, the single-cell layer that forms the lining of the small and large intestine.
The team from the MRC Human Immunology Unit (HIU), whose paper was published in the journal Nature, were supported by the NIHR Oxford Biomedical Research Centre.
Inflammatory Bowel Disease (IBD) affects at least 300,000 people in the UK, and its incidence is increasing worldwide, in particular in industrial-urbanised societies. There is no cure for IBD, and while many patients can manage the symptoms with appropriate care, around 40% of patients do not respond to available therapies.
Diseases such as IBD develop when the symbiotic relationship between the cells lining the surface of the gut wall and the trillions of bacteria that live inside the gut lumen breaks down.
Normally these bacteria are beneficial to our bodies, helping to digest food, training the immune system or preventing harmful bacteria from taking hold. However, in diseases such as IBD, the barrier cell layer that keeps these microorganisms inside the gut lumen breaks down, leading to emergence of harmful bacteria and subsequent inflammation.
To understand why this protective barrier breaks down, the MRC-HIU research team, led by Professor Alison Simmons, compared gut biopsies from healthy individuals and patients with IBD.

Rather than looking at these biopsies as a whole, inferring the average behaviour of different types of cell in each sample, the researchers were interested in examining each cell individually, to understand how each one is changed in disease.
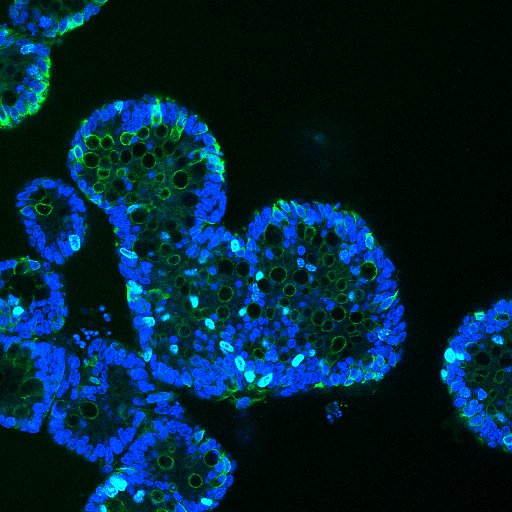
The team took advantage of the state-of-the-art single-cell facility at the MRC Weatherall Institute of Molecular Medicine to assemble a cell-by-cell map of the gut lining in health and IBD.
Using this careful analysis, researchers were able to identify a previously unknown sensor cell that can detect the level of acidity in the gut lumen.
They showed that these cells are located at the tip of the folds on the surface layer of the gut and secrete a hormone, uroguanylin, which regulates proliferation, metabolism and barrier function in the intestine on binding its ligand at acid pH. Surprisingly, these sensor cells were depleted in both IBD and colon cancer.
The researchers also examined the behaviour of barrier goblet cells. These cells play a pivotal role in secreting protective mucous over the colon surface to act as a block to an invasion of lumen bacteria.
Their analysis found several previously unknown subtypes of goblet cell, each with their own important function. The subtype that changed most dramatically in IBD normally produces an anti-bacterial substance. In IBD, this goblet cell type was damaged to such an extent, that it was unable to produce this anti-bacterial substance, leading to bacterial invasion and inflammation of the colon.
These results reveal a mechanism by which the gut stops being able to protect itself from luminal bacteria in patients with IBD.
This detailed analysis of the changes that happen to the gut in IBD opens new research opportunities; it provides the first insight, at single-cell level, of how the protective barrier of the gut keeps harmful bacteria at bay, and also how this barrier is disrupted in IBD.
“By identifying new colonic epithelial cell types and uncovering fundamental determinants of barrier breakdown in IBD we open up avenues to restore the protective mucus layer pharmaceutically” Prof Simmons, Professor of Gastroenterology in the Nuffield Department of Medicine, said.
“Our work is also the first time that we are able to understand how individual, single cells lining our gut change in inflammation and lose their ability to protect against the harmful effects of luminal microbes in IBD.”
As well as the Oxford BRC, this work was funded by the Medical Research Council, The Wellcome Trust and the NIHR.