 Researchers in Oxford have been awarded £1.8m in capital funding from the Department of Health and Social Care to expand their work to tackle the growing problem of antimicrobial resistance (AMR), including using whole genome sequencing to diagnose AMR.
Researchers in Oxford have been awarded £1.8m in capital funding from the Department of Health and Social Care to expand their work to tackle the growing problem of antimicrobial resistance (AMR), including using whole genome sequencing to diagnose AMR.
The funding was awarded to the NIHR (National Institute of Health Research) Oxford Biomedical Research Centre (BRC) to introduce new technologies for faster, more cost-effective sequencing of micro-organisms.
Antimicrobial resistance is the ability of micro-organisms such as bacteria or viruses, to stop antimicrobial drugs, such as antibiotics, antivirals and antimalarials, from working against it, rendering them ineffective.
The Oxford BRC laboratories are aiming to develop new vaccines that can tackle AMR in the NHS, as well as targeting common diseases for which antibiotics are often unnecessarily prescribed.
Better outcomes
“Whole genome sequencing for the diagnosis of AMR infections has real benefits for NHS patients, as it can quickly and accurately identify the best antibiotics to use. Not only does it lead to better patient outcomes, it also reduces the spread of AMR,” said Prof Derrick Crook, the Oxford BRC’s Antimicrobial Resistance and Modernising Microbiology Theme Lead.
“At present we have one small second-generation sequencer, so this purchase will increase our sequencing capability in Clinical Microbiology massively.”
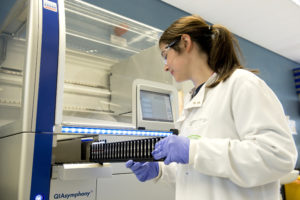 The funding has enabled the BRC and Oxford University Hospitals (OUH) to boost its ‘genome sequencing pipeline’ with the purchase of three genetic sequencing machines, which are located at the John Radcliffe Hospital, and powerful computers to analyse the results and store the findings. These are based at the John Radcliffe and the Big Data Institute, based at the University’s Old Road Campus, on the Churchill Hospital site.
The funding has enabled the BRC and Oxford University Hospitals (OUH) to boost its ‘genome sequencing pipeline’ with the purchase of three genetic sequencing machines, which are located at the John Radcliffe Hospital, and powerful computers to analyse the results and store the findings. These are based at the John Radcliffe and the Big Data Institute, based at the University’s Old Road Campus, on the Churchill Hospital site.
Two of the three sequencers are third-generation long-read sequencers, developed by Oxford Nanopore, a University of Oxford spin-out company.
Oxford is just one of four NIHR BRCs with a specific research theme devoted to infection/antimicrobial resistance. Last year, working with Oxford BRC, Public Health England launched the first national microbiology service in the world to routinely use whole genome sequencing, in this case for tuberculosis.
Sequencing
“This equipment will be used on samples, including from OUH patients, to better understand antibiotic resistance. Specifically we aim to improve diagnosis by using genetic sequencing instead of traditional lab-based clinical microbiology, so that clinicians learn more quickly and more accurately which antibiotic will be most effective on their patients, as we have done with tuberculosis,” Prof Crook said.
“It will also allow us to study how pathogens move between humans, farm animals and water courses, for example, and this will enable us to investigate potential outbreaks more effectively, as we’ll be able to determine if the infecting pathogens have a single source by comparing their genomes.”
A major focus of the work done my Oxford BRC is to control AMR by preventing infections caused by antibiotic-resistant bacteria through vaccination.
“We are developing vaccines that work against viruses, like flu and RSV, that can appear to doctors to be the same as dangerous bacterial infections and lead them to overuse antibiotics unnecessarily. The BRC has acquired state-of-the-art equipment to accelerate development of vaccines and monoclonal antibodies to combat AMR,” said Prof Andrew Pollard, Professor of Paediatric Infection and immunity at the University of Oxford, and the BRC’s Co-theme Lead for Vaccines for Emerging and Endemic Diseases
Transform
 Prof Pollard, head of the new AMR vaccines laboratory, said: “This new investment from NIHR will transform the pace of development of new vaccines and strengthen our capacity to overcome the dangers of resistant bacteria that threatens safety of patients in the NHS and are a major concern for global health security.”
Prof Pollard, head of the new AMR vaccines laboratory, said: “This new investment from NIHR will transform the pace of development of new vaccines and strengthen our capacity to overcome the dangers of resistant bacteria that threatens safety of patients in the NHS and are a major concern for global health security.”
The BRC has acquired two flow cytometers to allow it to expand the analysis of cellular responses to infection and vaccination, with a view to increasing the number of vaccines available and so reducing the need for antibiotic treatment. The machines allow for multiple samples to be analysed simultaneously in an automated way, rather than single samples having to be loaded manually as happens currently.
Also purchased were robots that allow the process of extracting DNA and RNA from samples from clinical vaccine trials to be automated, freeing up staff to do other tasks and giving more consistent results; and to process large numbers of patient samples quickly and consistently.
Prof Keith Channon, Director of Oxford BRC and of Research and Development at OUH, said: “This investment in the Oxford BRC gives a boost to our already excellent reputation as a leading centre of research in antimicrobial resistance, and increases our international reputation in this field.
“The cutting edge equipment will substantially increase the scale and speed with which we can generate and analyse AMR data, and that is great news for the NHS and its patients. This grant will allow us improve the capabilities for AMR research at Oxford University Hospitals and ensure that patients benefit from any breakthroughs that are achieved.”