A team of scientists at Oxford University’s Jenner Institute and Oxford Vaccine Group has taken the next step towards the discovery of a safe, effective and accessible vaccine against coronavirus.
The results of the Phase I/II trial, published today in The Lancet, indicate no early safety concerns and show the vaccine induces a strong immune response.
The vaccine provoked a T cell response within 14 days of vaccination and an antibody response within 28 days. T cells are white blood cells that can attack cells infected with the SARS-CoV-2 virus; antibodies are able to neutralise the virus so that it cannot infect cells when initially contracted.
Three leading members of the Oxford BRC’s Vaccines Theme are leading the trial: Prof Sarah Gilbert and Prof Adrian Hill of the University of Oxford’s Jenner Institute and Prof Andrew Pollard of the University’s Oxford Vaccine Group. The Oxford BRC provided crucial funding to get the trial up and running and then helped to fund an evaluation of the safety of the vaccine.
Booster
During the study, participants who received the vaccine had detectable neutralising antibodies, which have been suggested by researchers as important for protection, and these responses were strongest after a booster dose, with 100% of participants’ blood having neutralising activity against the coronavirus.

The next step in studying the vaccine is to confirm that it can effectively protect against SARS-CoV-2 infection.
“The Phase I/II data for our coronavirus vaccine shows that the vaccine did not lead to any unexpected reactions and had a similar safety profile to previous vaccines of this type,” Prof Pollard, a co-author of the study, said.
“The immune responses observed following vaccination are in line with what previous animal studies have shown are associated with protection against the SARS-CoV-2 virus, although we must continue with our rigorous clinical trial programme to confirm this in humans,
“We saw the strongest immune response in the 10 participants who received two doses of the vaccine, indicating that this might be a good strategy for vaccination,” he added.
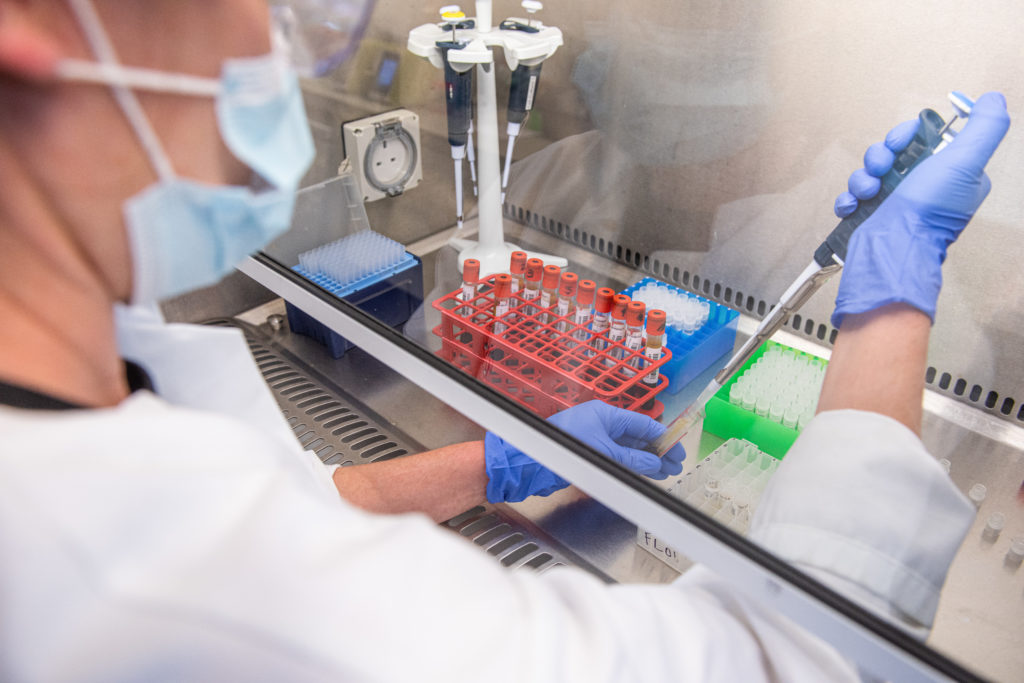
The team started working to develop a vaccine against the global threat of coronavirus in January 2020 and have been working with unprecedented urgency. A UK Phase I/II trial to test the Oxford ChAdOx1 nCoV-19 coronavirus vaccine began in April.
During the Phase I/II trial the vaccine has been evaluated in more than 1,000 healthy adult volunteers aged between 18 and 55 years in a randomised controlled trial. A subset of these volunteers (10 people) received two doses of the vaccine.
Encouraging
Between 23 April and 21 May, 1077 volunteers received the ChAdOx1 nCoV-19 vaccine or a placebo MenACWY vaccine. There were no serious adverse health events related to ChAdOx1 nCoV-19.
“These encouraging results support further evaluation of this candidate vaccine in our ongoing large-scale Phase III programme, that is still needed to assess the ability of the vaccine to protect people from COVID-19,” said Prof Gilbert, a co-author of the study.
The University of Oxford is working with the UK-based global biopharmaceutical company AstraZeneca for the further development, large-scale manufacture and potential distribution of the Covid-19 vaccine.
The project has been further spurred by £84 million of Government funding to help accelerate the vaccine’s development.
“We are encouraged by the Phase I/II interim data showing AZD1222 was capable of generating a rapid antibody and T-cell response against SARS-CoV-2. While there is more work to be done, today’s data increases our confidence that the vaccine will work and allows us to continue our plans to manufacture the vaccine at scale for broad and equitable access around the world,” said Mene Pangalos, Executive Vice President of BioPharmaceuticals Research and Development at AstraZeneca.
Global
Oxford and AstraZeneca are collaborating with clinical partners around the world as part of a global clinical programme to trial the Oxford vaccine. The global programme is made up of a Phase III trial in the US enrolling 30,000 patients, a paediatric study, as well as Phase III trials in low-to-middle income countries including Brazil and South Africa, which are already under way.
AstraZeneca remains committed to fulfilling their commitment for broad and equitable access to the vaccine, should late-stage clinical trials prove successful. So far, commitments to supply more than 2 billion doses of the vaccine have been agreed with the UK, US, Europe’s Inclusive Vaccines Alliance (IVA), the Coalition for Epidemic Preparedness (CEPI), Gavi the Vaccine Alliance and Serum Institute of India.
Business Secretary Alok Sharma said: “Today’s results are extremely encouraging, taking us one step closer to finding a successful vaccine to protect millions in the UK and across the world. Backed by £84 million Government investment for the vaccine’s development and manufacture, the agility and speed with which the University of Oxford have been working is outstanding. I am very proud of what they have achieved so far.”
Kate Bingham, Chair of the UK’s VaccineTaskforce said:“The UK is fortunate to have such outstanding academic innovators working alongside the highly experienced global team at AstraZeneca. This partnership is working at exceptional speed to demonstrate the safety and clinical effectiveness of the chadox vaccine in protecting people against COVID-19 infection.”
Developed at the Jenner Institute, ChAdOx1 nCoV-19, now known as AZD1222, uses a viral vector based on a weakened version of the common cold virus (adenovirus) containing the genetic material of SARS-CoV-2 spike protein.
After vaccination, the surface spike protein is produced, which primes the immune system to attack COVID-19 if it later infects the body. The recombinant adenovirus vector was chosen to generate a strong immune response from a single dose and it is not replicating, so cannot cause an ongoing infection in the vaccinated individual.
Vaccines made from the ChAdOx1 nCoV-19 virus have been given to more than 4,000 people to date and have been shown to be safe and well tolerated, although they can cause temporary side effects, such as a temperature, flu-like symptoms, headache or sore arm.
The potential vaccine entered Phase III clinical trials in May to study safety and efficacy in healthy volunteers aged 18 to 55 years across 19 trial sites in the UK. The University of Oxford is also working with research partners at a number of clinical trial sites around the world as part of this late stage trial.