Oxford researchers have developed a new method to quickly identify cancerous cells in babies at risk of leukaemia. The team hope that the new protocol could make rapid testing more accessible for clinical laboratories around the globe.
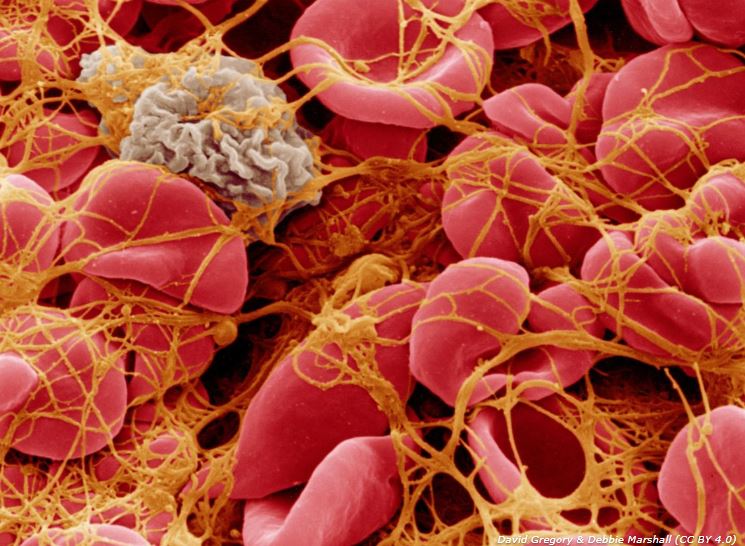
Until now, the only reliable way to know if a baby with Down’s syndrome is at risk of developing leukaemia, an aggressive form of blood cancer, was by a relatively expensive DNA mutational analysis of a blood sample.
Now, in a study published in the journal Blood, groups at the MRC Molecular Haematology Unit (MHU) have shown how they have developed an alternative, cheap method that quickly identifies cancerous cells.
The groups are led by the Professor Paresh Vyas, the Oxford BRC’s Co-theme Lead for Haematology and Theme Lead for Molecular Diagnostics, and by Prof Irene Roberts, of the University of Oxford’s Department of Paediatrics.
Babies with Down’s syndrome who have an alteration in the GATA1 gene have a remarkable propensity to develop a type of leukaemia known as ML-DS. Thirty percent of babies with Down’s syndrome have acquired mutations in the gene and 10% of them develop ML-DS before the age of five.
An altered GATA1 gene also causes a pre-leukemic disorder known as TAM, which in 20% of cases is fatal. It is important to identify babies with the genetic mutation who are at risk of developing ML-DS or who suffer of TAM to provide the best care possible.
Ideally, babies born with Down’s syndrome are tested at birth for GATA1 mutations by next-generation sequencing methods. Unfortunately, not all hospital laboratories can make use of this method, especially in developing countries, because it requires technical expertise and expensive equipment.
Instead of relying on DNA mutational analysis, the new approach developed by Profs Vyas and Roberts relies on flow cytometry, a method that is available in most haematology hospitals.

The value of this simple method comes from quick and easy identification of GATA1 mutant cells in blood samples from new-born babies.
It is hoped that one day most clinical laboratories around the world could make use of this method when next-generation sequencing methods are not available.
The GATA1 gene encodes two versions of a DNA binding protein important for healthy red blood cell and platelet production. These variants are known as GATA1fl and GATAs. Surprisingly, when mutations occur, they lead to exclusive expression of only GATA1s.
As well as the NIHR Oxford BRC, the research teams were funded by blood cancer charity Bloodwise, the MRC Molecular Haematology Unit, and Lady Tata Memorial Trust.