University of Oxford researchers have begun recruitment to a study looking at whether chemotherapy medication can reach pancreatic tumours more effectively if encapsulated within a heat-sensitive shell and triggered with focused ultrasound.
The Phase I PanDox study, which is supported by the NIHR Oxford Biomedical Research Centre (BRC), aims to learn if using thermosensitive liposomal doxorubicin and focused ultrasound (FUS) results in enhanced uptake of doxorubicin in pancreatic tumours, compared to doxorubicin alone.
PanDox is being carried out as a multi-disciplinary collaboration between the Oxford University Institute of Biomedical Engineering, the Oncology Clinical Trials Office (OCTO), Oxford University Hospitals (OUH) NHS Foundation Trust and Celsion corporation, the manufacturer of the proprietary heat-activated liposomal encapsulation of doxorubicin ThermoDox used in the study.

The Oxford BRC’s Co-theme Lead for Cancer, Prof Mark Middleton (pictured left), Head of the university’s Department of Oncology at is the chief clinical investigator on the trial. Prof Constantin Coussios, Director of the Institute of Biomedical Engineering, is the lead scientific investigator.
The trial will recruit 18 patients; ThermoDox will be administered intravenously in 12 patients with a pancreatic ductal adenocarcinoma tumour that cannot be removed with surgery; the drug will then be released by gentle heating produced by focused ultrasound outside the body. This will be compared to conventional systemic delivery of doxorubicin without FUS in the other six patients.
As well as assessing whether uptake of doxorubicin is improved with FUS, the team will compare how the tumour responds to the treatment, examine the impact on patient symptoms and assess the safety of the treatment.
The study, which is expected to be completed by December 2022, is similar in design to Oxford’s 10-patient TARDOX study, which demonstrated that ThermoDox plus focused ultrasound increased doxorubicin tumour concentrations by up to 10-fold and enhanced nuclear drug uptake in patients with liver tumours. The findings were published in Lancet Oncology.
The lead oncology clinical research fellow on the PanDox study, Dr Laura Spiers of OUH, said: “Pancreatic cancer has a low five-year survival rate of approximately 10% and drug-based treatments remain less effective than in other cancers, in part due to the unique challenges presented by the stroma surrounding pancreatic tumours.
“Therefore, finding innovative and effective means of delivering high concentrations of anti-cancer agents such as doxorubicin may lead to a breakthrough for this difficult-to- treat cancer.”
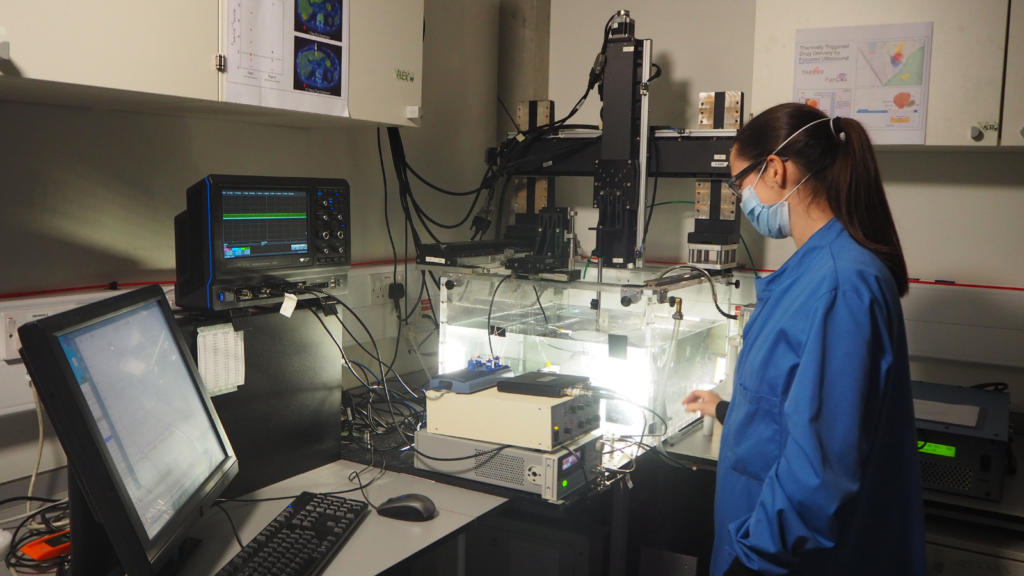
Dr Michael Gray, lead biomedical engineering research fellow, said: “Based on the patient-specific treatment planning approaches developed and validated during the TARDOX trial, PanDox will deliver focused ultrasound mild hyperthermia without either MR-based or invasive thermometry. The ultimate goal is to develop a cost-effective and scalable approach that can be rapidly deployed for the benefit of pancreatic patients.”