Replacing all regular meals with a low calorie diet of soups, shakes and bars, together with behavioural support, is cost-effective as a routine treatment for obesity, according to researchers from the University of Oxford.

Published today in the journal Obesity, the study is the first to estimate the long term health benefit and builds on the results of the DROPLET trial, which showed that ‘total diet replacement’ programmes (TDRs) are a safe and effective way to lose weight, with significant weight loss persisting to at least 12 months.
This study was funded by Cambridge Weight Plan Ltd, and supported by the National Institute for Health Research (NIHR) Oxford Biomedical Research Centre and the NIHR Collaboration for Leadership In Applied Health Research and Care (CLAHRC) Oxford.
Nearly two-thirds of adults in England are overweight or obese, increasing the risk of life-altering illnesses, such as type 2 diabetes, heart disease, stroke and some cancers.
The NHS recently announced a pilot programme to offer a TDR programme to around 5,000 people with type 2 diabetes and has also committed to offering weight loss support for people with hypertension who are also obese.
“Studies like ours, which provide reliable estimates of the long-term impacts of weight management programmes on patients’ health and healthcare costs, are of real importance to enable the NHS to select the most clinically and cost-effective services for their patients,” said lead author Dr Seamus Kent, of the University of Oxford’s Nuffield Department of Population Health.
Professor Susan Jebb, Professor of Diet and Population Health in University of Oxford’s Nuffield Department of Primary Care Health Sciences, Chief investigator of the DROPLET trial, said: “It is great to see the NHS Long Term Plan taking this research evidence and translating it into new clinical services for people who are obese.
“Our study provides great confidence that this programme is a cost-effective treatment, which could improve the health of large numbers of people who are affected by obesity.”
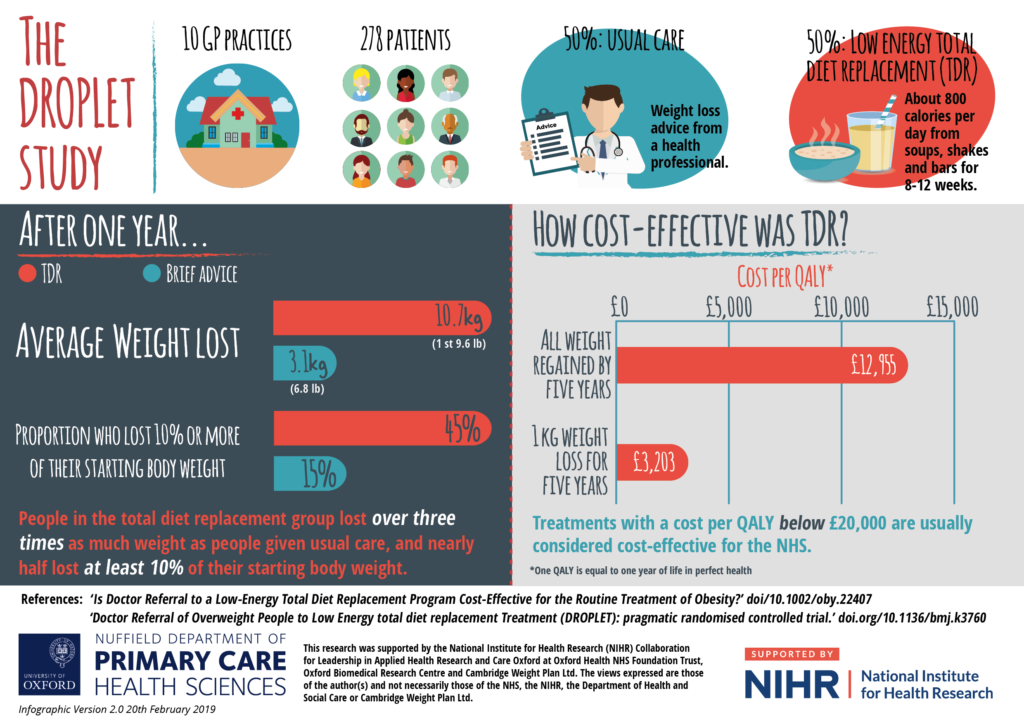
The NIHR-supported researchers compared a TDR programme with a nurse-led support programme, and made the conservative assumption that patients would regain any weight they lost due to the programme after five years.
The analysis estimated how many additional cases of common obesity-related conditions like type 2 diabetes, cardiovascular disease, and cancers would be avoided under the TDR programme, and the implications of this on the health of patients and healthcare costs.
They estimated that, for every 100,000 people referred to the TDR programme, 50 coronary heart disease events, 75 strokes, 900 cases of type 2 diabetes, and 25 cancers could be avoided. As a result, people are expected to live longer and in better health, with lower use and costs of healthcare services.
The TDR programme is expected to cost an additional £13,000 for every year of life lived in full health which is gained as a result of the treatment. In the UK, healthcare interventions are generally considered cost-effective if they provide such a benefit for less than £20,000.
“The DROPLET trial showed that after 12 months people on total diet replacements lost on average 10.7kg (1 stone, 9lb), which was 7.2kg (1 stone, 1 lb) more than those only receiving the standard nurse-led programme of weight loss advice,” said co-author Dr Nerys Astbury, of the University of Oxford’s Nuffield Department of Primary Care Health Sciences.
“This new analysis adds to that finding by strongly suggesting it’s also a cost-effective treatment for the NHS to offer, particularly in middle-aged and older adults.”