A glowing marker dye that sticks to prostate cancer cells could help surgeons to remove them in real-time, according to new research.
Scientists at the University of Oxford and Oxford University Hospitals NHS Foundation Trust, supported by Cancer Research UK and the NIHR Oxford Biomedical Research Centre (BRC), used a fluorescent dye attached to a special marker molecule to give doctors a ‘second pair of eyes’ during surgery for prostate cancer.
Twenty-three men with prostate cancer were injected with the marker dye before undergoing prostate removal surgery. The marker dye found areas of cancerous tissue not picked up by the naked eye or other clinical methods.
The dye allowed the surgeons to remove all cancerous tissues whilst preserving healthy tissues.
The combination of dye and targeting molecule, called IR800-IAB2M, allows surgeons to see the edges of the tumour and identify any clusters of cells that have spread from the tumour into nearby pelvic tissues and lymph nodes. This guides the surgeon to remove all cancerous tissues and preserve healthy areas around the prostate. This substantially reduces the chances that the cancer will come back in future and minimises the possibility of life changing side-effects for the patient after the operation.
The dye and marker molecule work by attaching themselves to a protein called prostate-specific membrane antigen (PSMA) commonly found on the surface of prostate cancer cells.
The marker molecule is made from a smaller version of an antibody called a ‘minibody’, which can only bind to PSMA and not to any other molecule. The dye and marker molecule combination were developed by Oxford scientists in collaboration with US company ImaginAb Inc.
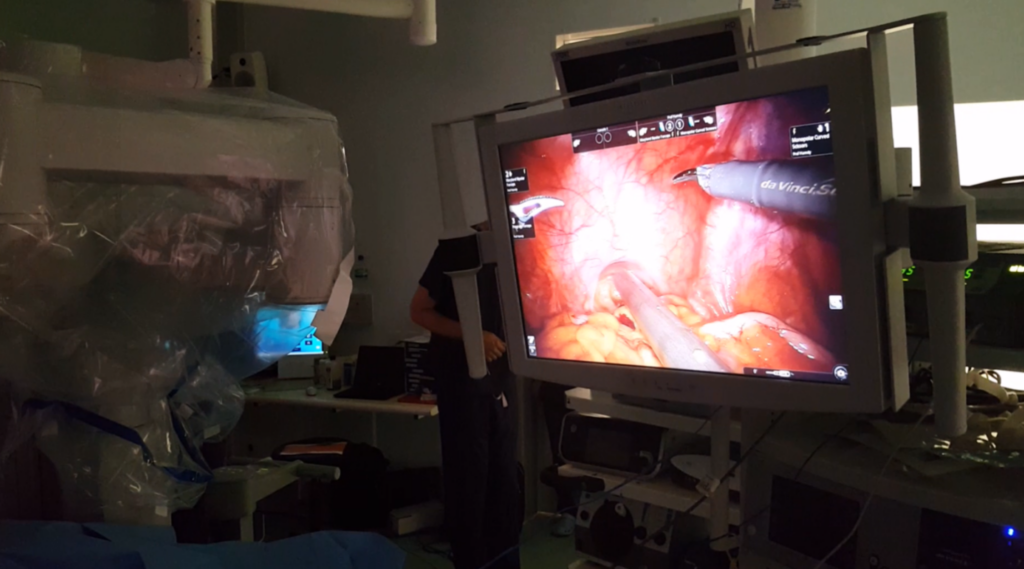
In the first stage of the ProMOTE study, published in the European Journal of Nuclear Medicine and Molecular Imaging, 23 men diagnosed with prostate cancer were injected with the fluorescent dye before undergoing robot-assisted surgery to remove the prostate, known as a radical prostatectomy. Surgeons used an imaging system that shines a special type of light on the prostate and nearby areas, to make the prostate cancer cells glow. The imaging system was developed by an engineering team led by Professor Borivoj Vojnovic at the University of Oxford.
For multiple patients in the study, the dye identified clusters of cells which had spread away from the tumour which couldn’t be seen by the naked eye. This marker dye is in its early stages of clinical development, but in future it could be used routinely by surgeons to see every part of the cancer while they perform surgery to remove the prostate.
The imaging system to see glowing cancer cells could be integrated into the robot-assisted tools used for prostate surgery. The marker dye could also be used for other types of cancer, by changing the protein it uses to attach itself to the cancer cells.
Further clinical trials are already underway in larger groups of patients to find out if the technique removes more prostate cancer, and preserves more healthy pelvic tissue, compared to existing surgical methods.
Prostate cancer is the most common cancer in men in the UK, with around 52,300 new cases every year.

Nuffield Professor of Surgery at the University of Oxford and lead author of the study, Professor Freddie Hamdy, said: “We are giving the surgeon a second pair of eyes to see where the cancer cells are and if they have spread. It’s the first time we’ve managed to see such fine details of prostate cancer in real-time during surgery.
“With this technique, we can strip all the cancer away, including the cells that have spread from the tumour which could give it the chance to come back later. It also allows us to preserve as much of the healthy structures around the prostate as we can, to reduce unnecessary life-changing side-effects like incontinence and erectile dysfunction.”
Professor Hamdy added: “Prostate surgery is life changing. We want patients to leave the operating theatre knowing that we have done everything possible to eradicate their cancer and give them the best quality of life afterwards. I believe this technique makes that possibility a reality.”
David Butler, a retired sales development manager from Southmoor in Oxfordshire, was one of the 23 men who took part in the study. A chance conversation with his GP turned into a shock diagnosis of prostate cancer in November 2018.
“I had literally no symptoms apart from needing to pee more quickly whenever I did go to the toilet. Had I not told my GP about it, I might not have caught my cancer until it was much further down the line.
“Very strangely, I was relaxed about the diagnosis. I had a sense that the consultant was going to tell me it was bad news – so I wanted to be positive and face up to it. I think the staff thought I was taking it extremely well!

“I had several biopsies and scans but one scan – the PSMA PET scan – revealed that the cancer was starting to spread from the prostate. It was in the lymph nodes, it was in loads of places near to the prostate. That information proved vital to the doctors to get the cancer treated quickly.”
David had his prostate removed, along with several lymph nodes and other cancerous tissues, using this revolutionary technique in January 2019. His road to recovery was rocky after suffering a stroke shortly after the surgery, due to an unrelated heart condition. Five years on, he is fully recovered and has been cancer-free ever since.
“If you’re not positive, life will come up and bite you, so you’ve got to enjoy every moment. I am a very lucky man to have had the life I’ve had. I’ve dealt with a lot health-wise but I’ve had excellent treatment too.
“I retired early to make the most of life’s pleasures – gardening, playing bowls and walking. Taking part in the ProMOTE study has allowed me to have many more of those pleasures for years to come.”