Defining and therapeutically targeting immune drivers of progressive lung fibrosis
Lead: Professor Ling-Pei Ho
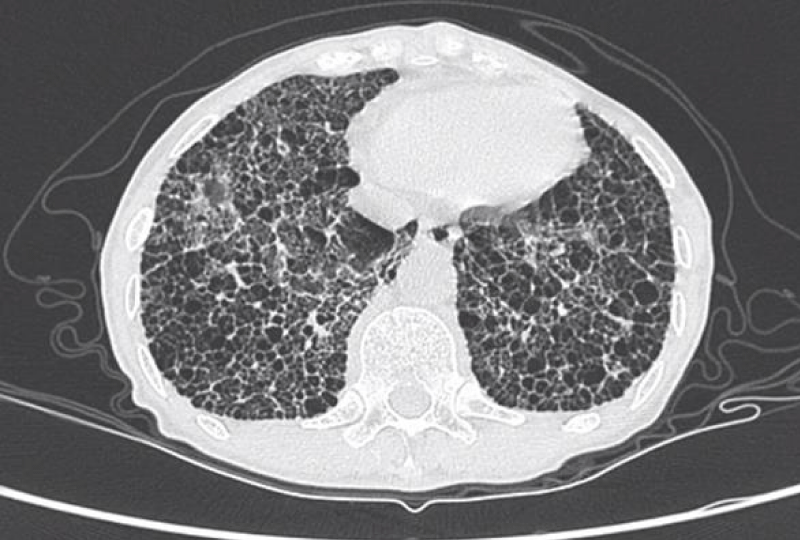
Lung fibrosis is excessive scarring and happens when normal healing process goes awry. The accumulation of scar tissue makes breathing more difficult. It happens not only in a condition called IPF (Idiopathic pulmonary fibrosis) but in other lung diseases such as fibrotic sarcoidosis.
We want to find out what causes the lungs to continue this ‘healing’ process and therefore understand the mechanism for the progression of fibrosis. We want to translate this knowledge into the development of new drugs for these patients. To do this, we will find markers in the blood and lungs that help us determine which patients are more likely to progress to fibrosis, so that we can treat these patients earlier. We are combining cellular and gene expression biomarkers with state-of-the-art hyperpolarised xenon MRI, to identify early disease in the lungs that precedes fibrosis.
In lung diseases, we have long focused on what happens in the blood to inform us of what new drugs to test. We now know that what happens in the lungs is often different to what happens in the blood, and so we are focusing on abnormalities in the lungs themselves, to help us understand the kind of targets we should be looking at for the next generation of drugs.
This tissue-informed therapeutic targeting will use the latest technologies in cell mapping that we have developed with our computational and mathematics colleagues. For example, our single cell mass cytometry imaging study is a new method of identifying abnormal cells in the lungs, where each cell in the lung can be identified with greater accuracy than ever before, pinpointing the proteins that can be targets for new drugs.
Working with our BRC’s Inflammation across Tissues theme, we are also carrying out innovative clinical trials that use modern statistical methods to test one drug on multiple but similar diseases. This, in combination with better understanding of the causes of disease and using biological and clinical outcome measures means we need fewer patients to conclude on the effectiveness of a new drug, and whether or not to proceed to later-phase trials. The first drug we are testing in this way is a CSF-1 receptor inhibitor which targets monocytes in IPF and fibrotic sarcoidosis.